As a Community Health Plan of Washington (CHPW) provider, you can count on our support in caring for your patients. Find answers to questions you may have about our provider portals, accessing training and orientation materials, and more.
How can I become a Community Health Plan of Washington Provider?
To join our network, please fill out and submit an online Provider Enrollment form. We will review your information and contact you within 30 days. If you have questions, please contact our Provider Relations department at [email protected].
How can I receive technical case management assistance?
Case managers are available to provide technical assistance to PCPs and Specialists for members with any condition. This support includes arranging referrals including mental health, SUD, Long Term Support Services and community support services. To access these services, contact the Case Management team at 1-866-418-7004.
Where can I find more information about using Jiva?
If you are new to using the Jiva portal, read our frequently asked question guide.
For portal-specific support, please contact [email protected].
How do I register for the HealthMAPS portal?
Register for HealthMAPS here. You need your Billing Tax ID number(s) to register. It may take up to 10 calendar days for your registration to process. You will receive an email when your registration is complete.
How do I know if a drug I prescribe is on the formulary?
You can review the formulary lists to identify what drugs are covered by CHPW and which require preauthorization. Drugs not listed on our formulary require prior authorization. You can submit prior authorization requests through our care management portal (Jiva.)
For self-administered drugs requiring prior authorization, please contact Express Scripts at 1-844-605-8168 or use https://www.CoverMyMeds.com to start the prior authorization process.
Who do I contact for claim status, prior authorization, member benefits, or member eligibility?
Providers can get in touch with their Provider Relations Representative or contact customer service for assistance at 1-800-440-1561.
I have a patient who missed their appointment without warning. Can I still bill them?
No. Patients cannot be billed for missed appointments. Make sure they are aware of your clinic’s cancellation or late appointment courtesy policies.
My patient needs to see an out-of-network specialist. Can I still refer them?
You may refer your patient to a non-networked provider without submitting a prior authorization request.
ChildrenFirst™ Rewards Program
Can a new pregnant member past their first trimester be eligible for the $60 prenatal gift card reward, or only the second visit $40 gift card?
If the member has had a prenatal visit within 45 days of enrolling in CHPW, they are eligible for the first $60 gift card. If they have a second prenatal visit, they are eligible for the second $40 gift card – they must have had a first visit to be eligible for the second visit card.
Can a new member who was not aware of their pregnancy until after first trimester, and just started prenatal care, claim the $60 prenatal gift card?
If they are a new member who has their first prenatal visit within 45 days of enrolling, they can claim the $60 gift card.
What if a member is pregnant with twins/triplets or learns they are pregnant with twins/triplets after their initial prenatal visit?
Members who are aware of a multiple pregnancy should select the “Twins” or “Triplets” option on the Prenatal Reward Request Form.
If a member has already submitted a request for their first prenatal visit and later learns that they are expecting twins/triplets, they should contact Customer Service to request additional prenatal rewards card(s).
What is the time requirement between Well Child visits?
The below Well Child visit milestones do not have a minimum time requirement between visits:
- Two Weeks
- 1 Month
- 2 Months
- 4 Months
- 6 Months
- 9 Months
- 12 Months
- 15 Months
- 18 Months
- 24 Months
- 30 Months
Annual Well Child visits, beginning at 3 years old, must take place at least 6 months apart to be eligible for the $20 gift card reward.
If member states they didn’t receive the gift card and the card has not been returned to CHPW, can a new one be issued? If so, how many times can a new card be issued if this continues to happen?
CHPW may approve a one-time reissue of a new card to members who did not receive their physical gift card via mail. Members must contact Customer Service so that we have a record of their request.
New, replacement cards may be issued up to (1) time per year per member.
How far back can a member claim a reward?
Reward card requests must be submitted no later than 6 months after the prenatal, postpartum, or well-child visit.
Requests submitted later than 6 months after the visit will not be approved.
Reminder: The member must be enrolled with CHPW at the time of visit to be eligible.
MemberFirst™ Rewards Program
What is the CHPW MemberFirst™ Rewards Program?
MemberFirst™ is CHPW’s new member incentives program created to encourage CHPW members to get preventive screenings.
Similar to the CHPW Apple Health (Medicaid) ChildrenFirst™ program, CHPW members can earn gift card rewards for completing recommended health services.
To claim rewards, eligible CHPW members fill out an online form after completing a qualified cancer screening.
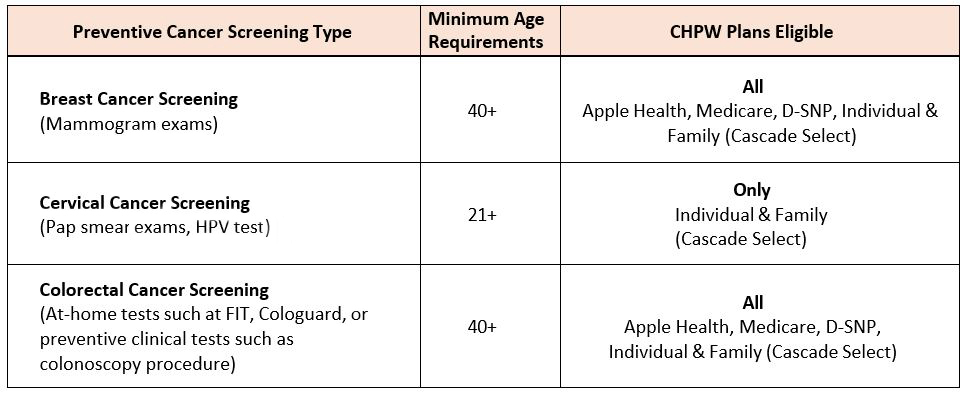
Which health services can CHPW members earn rewards for completing? Who is eligible?
Rewards are only available to current CHPW Members. They must meet the age requirements by screening type and be a CHPW member with the eligible plan at the time of the screening.
All CHPW health plans offer rewards for certain preventive screenings with MemberFirst™ rewards.
For CHPW Apple Health members, ChildrenFirst™ Rewards for prenatal, postpartum, and well-child checkups are also offered. For help with a member eligibility issue, email [email protected].
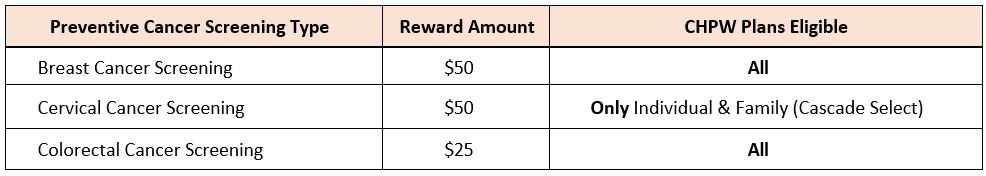
What is the reward for each screening and where can gift cards be used?
Reward amounts vary by screening type. Members choose a digital or physical card from Amazon, Albertsons/Safeway, Target.
How often can members earn MemberFirst™ rewards?
Once per year, per screening type, per eligible member. CHPW encourages members to talk to their doctor or health care provider about what type of screenings they should get and how often they should get them.
For Apple Health members, there is a $200 yearly limit for total rewards a member can earn.
Is there a cost for the screenings?
Most preventive screenings are covered by CHPW at no additional cost to members.
CHPW follows the regulatory bodies (HCA, Affordable Care Act (ACA), CMS) for preventive services and cost shares.
Visit healthcare.gov, cms.gov, and hca.wa.gov for details.
CHPW Provider Resources and Member Benefit Grids
How do members claim rewards?
It’s all online. Claim rewards within 180 days (about 6 months) of screening or test to qualify by filling out a “rewards submission form”.
In the form, members provide their member number, and information about the completed screening.
Where can members get more information and access the form to claim rewards?
Get answers to common questions and access the reward submission forms for CHPW members:
If you still have questions, call Customer Service for help. Our representatives are available at 1-800-440-1561 (TTY Relay: Dial 711) Monday through Friday, from 8 a.m. to 5 p.m.


