CHPW would like to remind all clinics and providers that claims must be billed with valid, appropriate taxonomy codes for the billing provider and, when applicable, the rendering provider.
CHPW’s clearinghouse has been rejecting any claims submitted without valid billing and/or rendering taxonomy codes and those claims are not submitted to CHPW.
A solo practice provider claim is only required to bill the NPI/taxonomy at the billing level as the billing provider and rendering provider are the same. If your billing provider name is different from your rendering provider name, then separate NPIs and taxonomies are required; in this case, the billing and rendering cannot be the same taxonomy code.
Electronic Billing of Taxonomy
- Billing Taxonomy goes in Loop 2000A, PRV*BI Segment (paper claims: Box 33b)
- Billing NPI goes in Loop 2010AA, NM1*85 Segment (Box 33a)
- Billing Tax Identification Number (TIN) goes in Loop 2010AA, REF*EI Segment (Box 25)
- Rendering NPI goes in Loop 2310B, NM1*82 Segment (Box 24j – bottom)
- For FQHCs, if the rendering provider is different than that in loop 2310B, enter taxonomy in the 2420A loop.
- Rendering Taxonomy goes in Loop 2310B, PRV*PE Segment (Box 24j – top)
See the “Electronic Claim Example” and “Paper Claim Example” sections at the end of this bulletin for visual representations.
Please continue reading for more information about taxonomy codes or see the NUCC’s Health Care Provider Taxonomy Code Set to find other taxonomies that may be applicable.
Tribal Providers
Tribal providers must bill with the appropriate billing taxonomy and the appropriate assigned American Indian/Alaskan Native (AI/AN) or non-AI/AN tribal modifier.
Acceptable Taxonomies for Tribal Providers
- Medical claims: 208D00000X, 225100000X, 225X00000X, 235Z00000X, 152W00000X, 171M00000X, and 174400000X
- Mental health claims: 2083P0901X
- Substance use disorder claims: 261QR0405X
- If billing code H0020, you must also bill 261QM2800X as the rendering/servicing provider; refer to the Washington State Health Care Authority (HCA) Substance Use Disorder (SUD) Billing Guide for more information
- Residential treatment facilities: 324500000x or 3245S0500x
Please refer to the HCA Tribal Health Billing Guide for details.
Behavioral Health Services
For CHPW Behavioral Health Services Only (BHSO) plan/members (Behavioral Health Administrative Services Organization (BH-ASO) clients), the HCA is responsible for payment of services that are considered lower level acuity care. Professional behavioral health claims for such services should be submitted through ProviderOne. The HCA will determine payment on the following criteria:
- If the provider is a Community Mental Health Center, taxonomies 251S00000X or 261QM0801X, the reimbursement is the responsibility of the managed care organization (MCO) and will be denied by HCA informing the provider to bill the MCO/BH-ASO.
- The following billing taxonomies indicate behavioral health services and are the responsibility of the MCO/BH-ASO: 261QR0405X, 261QM2800X, 324500000X, 3245S0500X, 261QM3000X, 2083P0901X, 261QM0850X, 320800000X, and 323P00000X.
- Taxonomy 283Q00000X for psychiatric hospital should be billed to the MCO/BH-ASO.
- CHPW will deny claims for any billing taxonomies other than those listed in #1-#3 above. HCA considers other taxonomies to be for lower acuity services and will process and pay as a medical claim, versus a behavioral health claim, no matter the diagnosis. The HCA only looks at the billing taxonomy.
- The HCA will only pay for services that are covered through fee-for-service; services that are not covered through fee-for-service should be billed directly to the MCO, regardless of taxonomy.
- Please see the HCA Mental Health Services Billing Guide regarding appropriate billing and use of taxonomies.
- The HCA will escalate any future identified billing errors by providers to the HCA’s Program Integrity staff.
All behavioral health services must be billed with the appropriate billing taxonomy, including but not necessarily limited to, those listed below.
- Community Mental Health Centers: 251S00000X or 261QM0801X
- Behavioral health agencies (billing provider): 261QR0405X, 261QM2800X, 324500000X, or 3245S0500X
- Rehabilitation (rehab) for substance use disorder (SUD): 261QR0405X
- Methadone clinic/center: 261QM2800X
- SUD rehab facility: 324500000X
- Children’s SUD rehab facility: 3245S0500X
Rural Health Clinics (RHC)
RHC services must be billed with the RHC taxonomy in order to receive the service-based enhancement (SBE). As specified in the HCA’s Rural Health Clinics Billing Guide:
How do I bill taxonomy codes for RHCs?
-
- When billing for services eligible for an encounter payment, HCA requires RHCs to use billing taxonomy 261QR1300X at the claim level.
- A servicing taxonomy is also required.
- If the client or the service does not qualify for an RHC encounter, RHCs may bill regularly as a non-RHC without HCPCS T1015 on the claim.
Please refer to the HCA Rural Health Clinics (RHC) Billing Guide for more information.
Federally Qualified Health Centers (FQHC)
As a best practice, CHPW follows the HCA’s billing requirements for FQHCs. As specified in the HCA’s Federally Qualified Health Centers (FQHC) Billing Guide:
How do I bill taxonomy codes for FQHCs?
- When billing for services eligible for an encounter payment, HCA requires FQHCs to use billing taxonomy 261QF0400X at the claim level.
- A servicing taxonomy is also required.
Please see the “Electronic Billing of Taxonomy” section of this topic (above) or refer to the HCA Federally Qualified Health Centers (FQHC) Billing Guide for more information.
Applied Behavioral Analysis (ABA) Taxonomy
Applied Behavioral Analysis (ABA) providers must use taxonomy number 103K00000X for billing ABA therapy services to ensure claims are paid appropriately. This is the only applicable, reimbursable taxonomy for ABA CPT codes. Providers must enter this taxonomy code in both the billing and the servicing taxonomy fields on the CMS-1500 (HCFA) claim form.
Please see the NUCC’s Health Care Provider Taxonomy Code Set for more information.
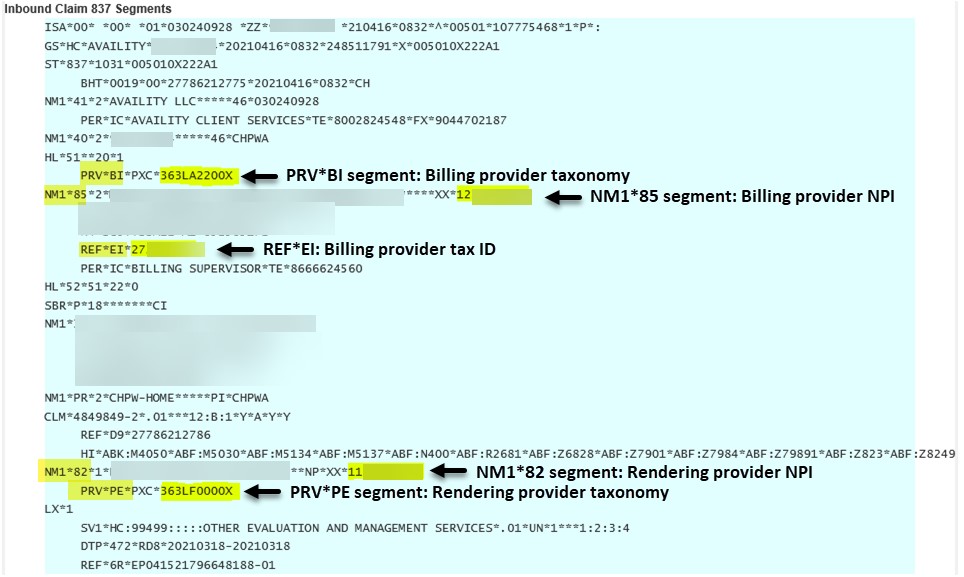
Electronic Claim Example
In the individual provider electronic claim example below:
• PRV*BI segment is the billing provider taxonomy
• NM1*85 segment is the billing provider NPI
• REF*EI segment is the billing provider Tax ID
• NM1*82 segment is the rendering provider NPI
• PRV*PE segment is the rendering provider taxonomy
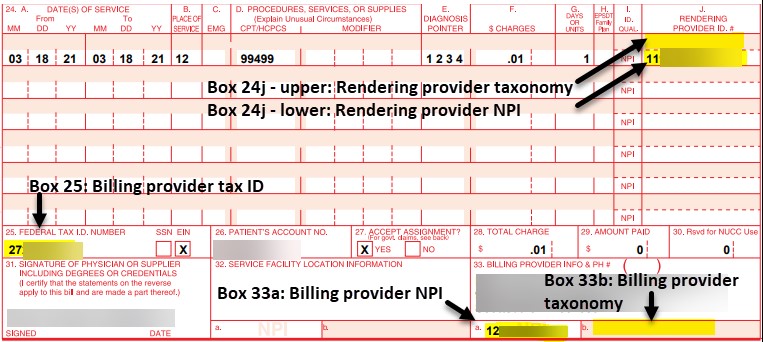
Paper Claim Example
In the individual provider paper claim example below:
-
-
-
- Box 24j – upper is the rendering provider taxonomy
- Box 24j – lower is the rendering provider NPI
- Box 25 is the billing provider Tax ID
- Box 33a is the billing provider NPI
- Box 33b is the billing provider taxonomy
-
-
Billing Guides
Please see the HCA Billing Guides for accurate taxonomies and more information, including the Tribal Health Billing Guide, Federally Qualified Health Centers (FQHC) Billing Guide, Rural Health Clinics Billing Guide, and more.
Questions?
If you have questions about the information in this bulletin, please contact EDI Support at [email protected]. If you are inquiring about a specific claim/rejection, please include the claim number, member ID, date of service, and billed charges as this will aid in our research to resolve the rejection from the clearinghouse.


